Accuracy of Pedicle Screw Placement remains a Critical Issue in Spine Surgery
Pedicle screw-based stabilization is the gold standard for treating spinal instabilities and deformities. Technological advancements such as Screws in the Thoracic Spine, Cortical Bone Trajectory and Minimally Invasive Surgery are compounding the importance of pedicle screw placement.
20% of pedicle screws have been reported as misplaced when using conventional techniques and around 5% when using navigation1-2.
Consequences of Misplaced Pedicle Screws are not to be Underestimated.

Complications of Misplaced Screws
Neurological Symptoms
3.7%
of the patients on average experience neurological symptoms after a spine surgery
(from 0% to 11%)3-16.
Revision Surgery
4.4%
of the patients on average have a revision surgery to correct a misplaced screw
(range 1% to 11%)3-16.
High Risk of Reoperation
2nd
cause of reoperation within 30 days of spine surgery in patients is due to neurological complications after posterior lumbar instrumentation and/or in trauma patients16.
Costly
$17,650
to $27,768 additional cost for a revision surgery to correct misplaced screw17-20.
Misplaced screws can happen to anyone
Misplaced pedicle screws can happen to anyone and can have serious consequences for the patient, for you, and for the hospital. Dr. Randal Betz explains why he believes PediGuard with DSG Technology helps ensure accurate pedicle screw placement and should be standard of care in spinal fusion procedures.
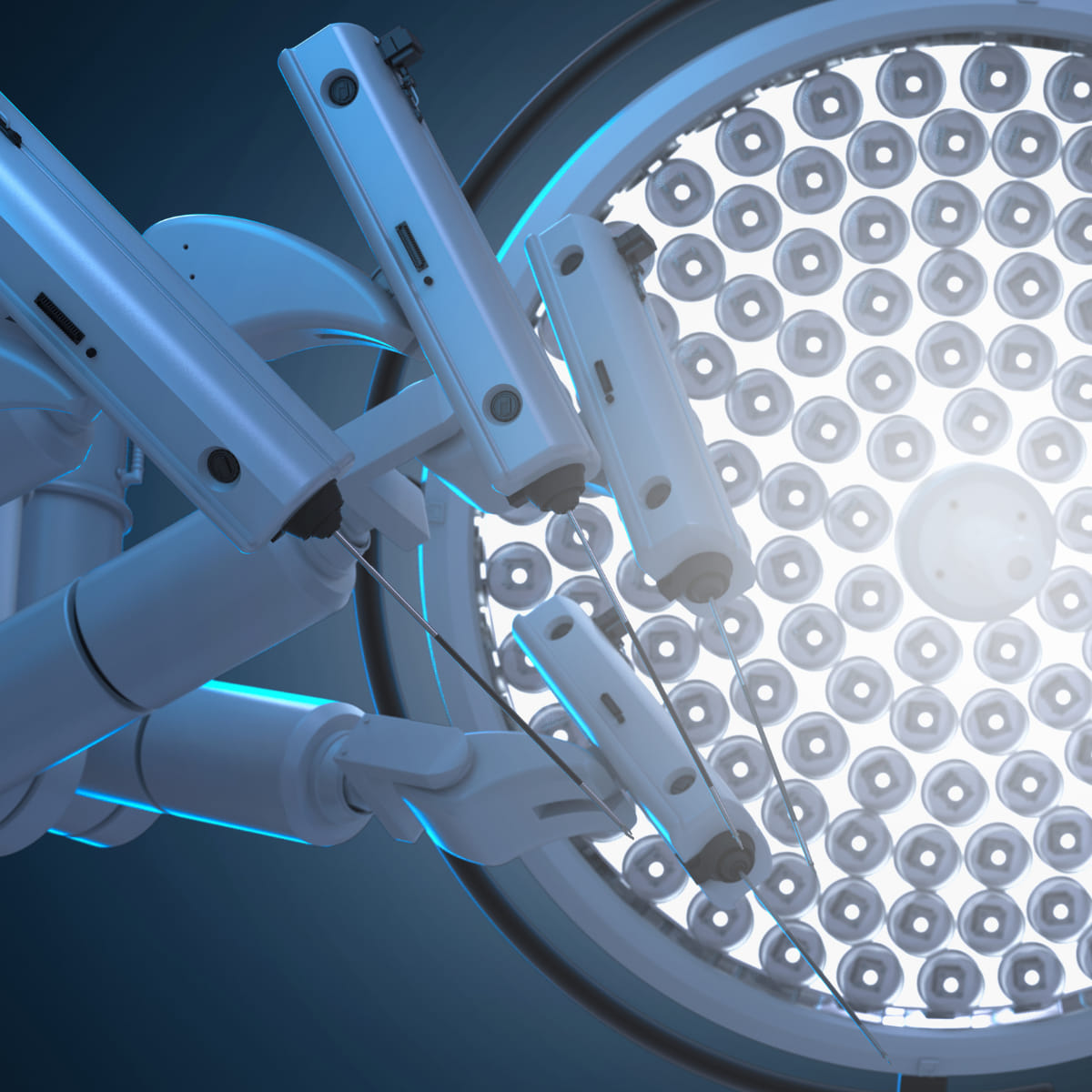
Robotics and Navigation are not perfect
While navigation and robotic surgery potentially offer better outcomes, they are not without drawbacks.
Intraoperative navigation increases radiation exposure to patients especially in AIS. When accounting for clinical and radiographic differences, patients treated with intraoperative navigation received 8.18 mSv more radiation. It is projected that intraoperative navigation will generate approximately one iatrogenic malignancy for every 1,000 AIS patients treated23. Rates of pedicle screw perforation are influenced by distance from the reference frame in multilevel registration using a CT-based navigation system during scoliosis procedures. A distance of three vertebrae or more above or below the reference frame vertebra produced significantly more frequent perforations. See below for other potential drawbacks with robotic and navigation platforms.
- High initial capital cost of robotic platforms (as high as $1.5M22) as well as ongoing consumables puts them out of reach for many smaller institutions.
- Clinical superiority has not yet been shown vs. freehand5.
- Rate of misplaced screws for robotics is still as high as 5%1-2.
- Does not rely on real-time imaging.
- Overreliance on robotics & navigation may erode surgeon skill and presents risks during a malfunction21.
We are committed to making spine surgery safer, especially in robotics. See our promising study results for robotics incorporating our DSG Technology.
How DSG Technology can help
Accurate
97% pedicle screw placement accuracy24-31
Anticipate breach
98% overall breach detection32
Time savings
15% surgical time reduction27
Less radiation
73% reduction in MIS procedures33
References
1 – Mason A et al. J Neurosurg Spine. 2014 Feb;20(2):196-203.
2 – Shin BJ et al. J Neurosurg Spine. 2012 Aug;17(2):113-22. Epub 2012 Jun 22.
3 – Amato V et al. J Neurosurg Spine. 2010 Mar;12(3):306-13.
4 – Amiot LP et al. Spine 2000 Mar 1;25(5):606-14.
5 – Waschke A et al. Eur Spine J. 2013 Mar;22(3):654-60.
6 – Sarlak A et al. Eur Spine J. 2009 Dec;18(12):1892-7. Epub 2009 Jun 14.
7 – Oh HS et al. Spine J. 2013 Dec;13(12):1751-7.
8 – Koktekir E et al. Spine J. 2014 Apr 3.
9 – Nevzati E et al. World Neurosurg. 2014 Jun 17.
10 – Kerry G et al. J Craniovert Jun Spine [serial online] 2014.
11 – Krauss M et al. Global Spine J. Dec 2014
12 – Du JY et al. Bone Joint Res. 2016 Feb;5(2):46-51.
13 – Verma SK, Singh PK, Agrawal D, Sinha S, Gupta D, Satyarthee GD, Sharma BS. O-arm with navigation versus C-arm: a review of screw placement over 3 years at a major trauma center. Br J Neurosurg. 2016 Dec;30(6):658-661. Epub 2016 Jul 25.
14 – Kaliya-Perumal AK et al. BMC Musculoskelet Disord. 2017 May 30;18(1):229.
15 – Fichtner et al. World neurosurgery. September 2017.
16 – Shimizu T et al. Eur Spine J. 2015 Jul 14.
17 – Hodges SD et al. Orthopedics. 2012 Aug 1;35(8):e1221-4.
18 – Watkins RG et al. Open Orthop J. 2010 Aug 6;4:228-33.
19 – Sanborn MR et al.. Neurosurg Focus. 2012 Jul;33(1):E12
20 – Dea N et al. The Spine Journal. Published Online: October 06, 2015
21 – Spine surgeons spotlight 4 key issues with robots (beckersspine.com)
22 – Spine Surgery Robots Market Size To Hit USD 537.36 Mn By 2032 (precedenceresearch.com)
23 – BM Striano et al. Spine J. 2024 Jun;24(6):1087-1094
24 – Suess O, Schomacher M. Advances in Medicine. 2016;2016:4296294. doi:10.1155/2016/4296294.
25 – Defino H et al. Coluna/Columna. 2020;19(3):189-93
26 – Heimen K. DWG meeting 2014
27 – Bai YS et al. J Spinal Disord Tech. 2013 Aug;26(6):316-20.
28 – Chaput C et al. Prospective, Spine 2012 Oct 15; 37(21): E1314–E1321.
29 – Chang V et al. Poster, AANS 2009
30 – Lubansu A et al. Belgian Society of Neurosurgery annual meeting, Leuven, Belgium, March 2006
31 – Bocquet Jean-François and Violas Philippe. EuroSpine Annual Meeting. Istanbul, Turkey. 28-25 Oct. 2006. IMAST Annual Meeting. Athens, Greece. 12-15 Jul. 2006. Poster presentation.
32 – Bolger C et al. Eur Spine J. 2007 Nov;16(11):1919-24
33 – Lubansu A et al. EurosSpine 2011
For any request, don't hesitate to contact us